If you only have 5 seconds:
About ten minutes of cold water immersion and one hour of sauna per week, all spread over 2 to 3 sessions, can improve your metabolism, your thermoregulation and your sleep.
Otherwise, let’s dive deeper…
Winter swimming is popular in the Scandinavian and Baltic countries as well as in Finland. This practice involves immersing yourself for short periods, ranging from one to a few minutes, in the very cold water of an artificial pond, lake or ocean. In general, these immersions are associated with stays in a sauna. Fans of the practice, who we will call winter swimmers, say they do it for their health and popular wisdom says that they are sick less often. In this blog post, we will not cover the issue of cold and the immune system. Let us simply ask the following question: given that winter swimmers exercise themselves with extreme cold and heat, can we assume that they regulate their internal heat differently in response to the outside temperature? In other words: do they have a more efficient thermoregulation? What would be the impact of such an adaptation on their metabolism? These are the questions asked by researchers based in Denmark, with in mind the interest that such a practice can have in countering the progression of the metabolic syndrome – diabetes, obesity, cardiovascular problems, etc. – in the population (Søberg et al., 2021). The study consisted of measuring thermoregulation in a small cohort, 7 winter swimmers and 8 controls, homogeneous in terms of sex, age, BMI and VO2max. At the time of the study, winter swimmers had been exposed to the cold-and-sauna practice for at least one season, at the rate of 2-3 times a week.
First, a blood sugar test showed better insulin sensitivity in winter swimmers than in the control group, tending to confirm observations from previous studies. In addition, a stress test to assess activation of the sympathetic nervous system in response to cold – the test involved dipping the hand in 4˚C water for 3 minutes – showed less activation in winter swimmers, and therefore a presumed better acclimatization to the cold. Such preliminary observation remained to be confirmed in a general cold exposure test, cooling the entire body using temperature-controlled blankets.
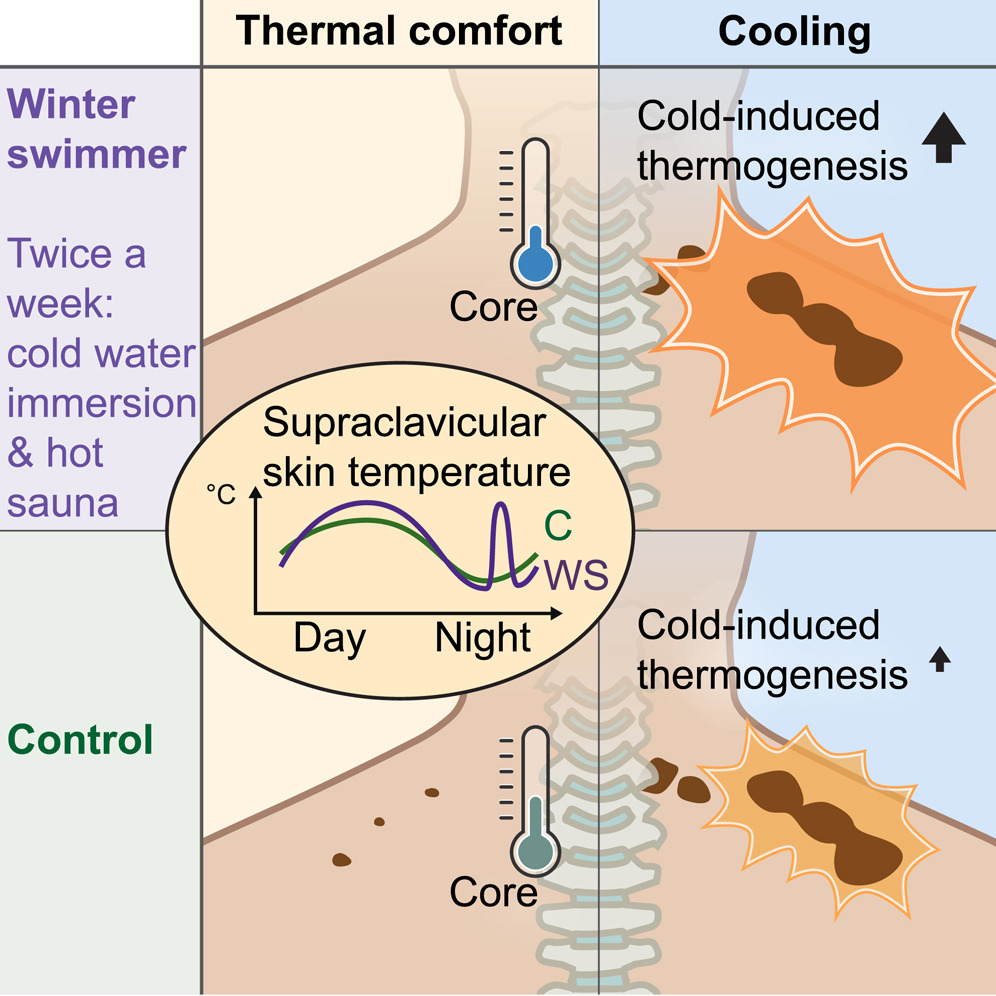
In particular, these experiences highlighted that winter swimmers seem to dissipate their internal heat more efficiently. In fact, their temperature is higher in the sternum and on the periphery of the body than in the control subjects. This thermoregulation is said to be a consequence of regular sauna use. In addition, during the body cooling test, the researchers observed that the winter swimmers produced more heat in the supraclavicular region than the people in the control group. This observation can be correlated with a greater energy expenditure of winter bathers during body cooling. The origin of this supraclavicular heat may well lie in the activation of brown fat. Brown adipose tissue, also called brown fat, is made up of adipocytes, cells rich in lipid reserves, the activity of which releases thermal energy instead of chemical energy (in the form of ATP) like their counterparts in white fat. Next, the researchers showed, in all subjects (winter bathers and controls), that the brown fat in the neck and diaphragm was activated upon exposure to the cold. On the other hand, at a comfortable temperature, a residual activity of the brown fat is detected in the witnesses but completely absent in the winter bathers. This phenomenon can be attributed to a difference in the perception of the comfort temperature threshold by immersions in cold water, or to a lower internal temperature resulting from stays in the sauna.
Heat production, especially in the supraclavicular region, does not come exclusively from the activity of brown fat. Indeed, muscle thermogenesis seems to add its contribution. In particular, the intercostal muscles can generate heat, and this was also observed in winter swimmers in this study. It will be noted here that intercostal muscle thermogenesis was observed in Wim Hof as being more important than the contribution of brown fat (Muzik et al., 2018). In addition to brown fat activity and muscle thermogenesis, white fat may participate. It appears that winter swimmers exhibit different lipid utilization, as highlighted by the gene expression of lipolysis markers in white fat.
The final question the study authors asked was about the diurnal regulation of body temperature. The latter is admittedly relatively stable, around 37˚C, but it actually varies slightly, dropping of 0.5˚C to 1˚C during the night. Over the entire 24-hour cycle, winter swimmers have slightly, but significantly, lower body temperatures than the control group. A lower internal temperature could promote better sleep. A low cortisol level at night is associated with better sleep. And precisely, the cortisol profile of the winter swimmers is lower during the night than that of the control. According to the authors, it is possible that the increase in cortisol at the end of the night triggers the activation of brown fat before awakening, in winter swimmers, in whom an intriguing increase in supraclavicular temperature is observed before waking up. The profile of interleukin-6 is also interesting because it is associated with certain phases of sleep and it was observed as different in winter swimmers. Finally, it should be noted that no difference between the winter swimmers and the control group was detected in terms of the number of red or white blood cells, although this is a point regularly put forward on the benefits of the cold.
Like any scientific study, this one has its limitations. The most important are the small sample (7 subjects per group) composed only of healthy men. So, it is difficult to know if we can extrapolate to the whole population. Among the delicate questions, one cannot know at this stage whether the physiological differences observed are the result of the practice or if physiological differences predispose to such a practice. One of the winter swimmers was withdrawn from the study because he did not respond to the brown fat activation test. This raises the question of non-brown-fat-based thermoregulation. Indeed, with one in seven subjects having such a profile, it can ultimately concern a lot of people. And we can point that brown fat seems to play a very modest role in a famous enthusiast of exposure to cold, namely Wim Hof (Muzik et al., 2018). Finally, it should be emphasized that the people studied, namely the winter swimmers, practice both cold water immersion and sauna. Therefore, this calls for caution before extrapolating these data for people practicing only one of the two activities.
To summarize briefly, this study showed that winter bathers tend to dissipate their body heat more and have a lower internal temperature. This would be associated with a lower than average comfort temperature. In addition, they generate more heat when subjected to cold, thus being more efficient in warming up, by activating the thermogenesis of brown adipose tissue and intercostal muscles. Finally, there are signs of better insulin sensitivity and improved quality of sleep. The authors of the study conclude that this practice could be of interest as a support in the fight against obesity. On a practical level, this consists of setting up about ten minutes of immersion in cold water and one hour of sauna per week, in 2 to 3 sessions. Even though this study may not prove that the combination of cold water and sauna will cure all ailments on Earth, it still adds nicely to the clues pointing this simple practice as beneficial for health.
🔥❄️🧠✌️
Sébastien.
References:
Muzik O, Reilly KT, Diwadkar VA. “Brain over body”-A study on the willful regulation of autonomic function during cold exposure. Neuroimage. 2018 May 15;172:632-641. doi: 10.1016/j.neuroimage.2018.01.067. Epub 2018 Feb 10. PMID: 29438845.
Søberg S, Löfgren J, Philipsen FE, Jensen M, Hansen AE, Ahrens E, Nystrup KB, Nielsen RD, Sølling C, Wedell-Neergaard AS, Berntsen M, Loft A, Kjær A, Gerhart-Hines Z, Johannesen HH, Pedersen BK, Karstoft K, Scheele C. Altered brown fat thermoregulation and enhanced cold-induced thermogenesis in young, healthy, winter-swimming men. Cell Rep Med. 2021 Oct 11;2(10):100408. doi: 10.1016/j.xcrm.2021.100408. PMID: 34755128; PMCID: PMC8561167.

Sébastien Zappa, PhD
Oxygen Advantage Master InstructorREBO2T – Practitioner
Wim Hof Method Instructor Level 2
ELDOA Practitioner Level 2
Overall Breathing & Cold Geek, Homo cryopulmosapiens…
Happy to coach you since 2018